Lyme Disease in Teens in America 2025
Lyme disease continues to pose a significant health threat to American teenagers, with the condition affecting hundreds of thousands of young people annually across the United States. As the most commonly reported tick-borne illness in the nation, this bacterial infection caused by Borrelia burgdorferi has shown persistent patterns of infection among adolescent populations, particularly those residing in high-incidence states spanning the Northeast, Mid-Atlantic, and upper Midwest regions. The disease’s prevalence among teenagers stems from their increased outdoor activity levels during peak tick season, combined with participation in recreational activities such as hiking, camping, sports, and outdoor socializing that elevate exposure risk to infected blacklegged ticks.
Understanding the current statistics and trends of Lyme disease in teenagers has become increasingly urgent, especially with recent groundbreaking developments in early detection. In November 2025, a team of high school students from Lambert High School in Georgia made headlines when they developed a revolutionary CRISPR-based diagnostic test that can detect Lyme as early as two days after infection – far sooner than the two weeks with existing tests. This breakthrough, if validated through further testing, could transform outcomes for teens and all Americans facing this debilitating illness. The adolescent years represent a critical period where outdoor engagement peaks, yet awareness about tick-borne disease prevention often remains insufficient, making innovations like the Lambert students’ work particularly vital for protecting this vulnerable age group.
Interesting Facts About Lyme Disease in Teens in the US 202
| Fact Category | Statistic | Details |
|---|---|---|
| Total US Cases 2023 | 89,000+ cases | Reported Lyme disease cases nationwide through surveillance |
| Estimated Actual Annual Cases | 476,000 cases | True burden including diagnosed and treated cases |
| Peak Pediatric Age Group | Ages 5-14 years | Highest infection rates among children and early teens |
| Teen Age Range Affected | Ages 10-19 years | Adolescent demographic showing elevated incidence |
| Male Predominance 2022 | 57.3% male cases | Gender distribution favoring males across all ages |
| High-Incidence States | 15 states | States consistently reporting elevated case numbers |
| Geographic Concentration | 95.5% | Percentage of cases from high-incidence jurisdictions |
| Daily Pediatric Cases | 200+ daily cases | Among children and teens due to outdoor exposure |
| Untreated Arthritis Risk | 60% | Patients developing joint complications without treatment |
| Neurologic Manifestations | 15% | Untreated patients experiencing neurological symptoms |
| Current Detection Window | 2+ weeks | Minimum time before standard antibody tests work |
| New CRISPR Detection | 2 days | Breakthrough early detection developed by teens in 2025 |
Data Source: Centers for Disease Control and Prevention (CDC), National Notifiable Diseases Surveillance System (NNDSS), 2022-2023 Reports; CBS News, November 2025
The statistics reveal the substantial burden Lyme disease places on teenage populations throughout America. The 89,000+ reported cases in 2023 represent only what gets captured through official surveillance channels, while CDC estimates suggest approximately 476,000 Americans are actually diagnosed and treated annually when including clinical diagnoses that don’t meet strict reporting criteria. This massive underreporting gap of more than five times the official count highlights serious challenges in current surveillance systems and confirms that actual teen infections substantially exceed reported figures. The 57.3% male predominance among documented cases reflects behavioral patterns where boys and young men typically engage in higher-risk outdoor activities more frequently than their female counterparts.
The finding that children aged 5-14 years represent the highest pediatric infection rate holds particular significance for teenagers, as this range encompasses early adolescence when outdoor recreational participation peaks. The bimodal age distribution consistently observed in national surveillance data confirms teens fall within the first major infection peak, emphasizing their vulnerability during these critical developmental years. Perhaps most alarming, the statistic showing 60% of untreated patients develop arthritis complications underscores why the Lambert High School students’ breakthrough matters so profoundly. Their CRISPR-based diagnostic that can detect Lyme as early as two days after infection could prevent the long-term joint damage, neurological complications, and cardiac problems that currently plague thousands of teens who don’t receive timely diagnosis and treatment with current testing methods that require waiting two weeks or longer before accurate results become possible.
Age Distribution of Lyme Disease Cases in Teens in the US 2023
| Age Group | Incidence Pattern | Key Characteristics | Risk Level |
|---|---|---|---|
| Ages 5-9 | Highest pediatric peak | Primary childhood infection peak, outdoor play exposure | Very High |
| Ages 10-14 | Continued elevation | Early teen years, increased independence outdoors | High |
| Ages 15-19 | Sustained high rates | Older adolescents, camping, hiking, sports participation | High |
| Ages 5-14 combined | Bimodal first peak | Encompasses early to mid-adolescence in distribution | Very High |
| Male teens (5-19) | Higher incidence | Boys demonstrate significantly elevated rates | High |
| Female teens (5-19) | Moderate-high incidence | Lower than males but still substantial disease burden | Moderate-High |
Data Source: CDC Surveillance for Lyme Disease, 2022-2023; National Notifiable Diseases Surveillance System
The age distribution data reveals critical infection patterns affecting teenagers across different developmental stages in the United States. The ages 5-9 group consistently demonstrates the highest pediatric infection rates nationwide, establishing a concerning pattern that continues through early adolescence. This peak reflects increased time spent outdoors during formative years combined with potentially lower awareness of tick-bite prevention measures among younger children transitioning into teenage years. The ages 10-14 bracket maintains significantly elevated incidence levels, capturing the critical early teenage period when independence grows and participation in outdoor recreational activities intensifies without necessarily corresponding increases in protective behaviors or tick awareness.
For older adolescents aged 15-19 years, surveillance data indicates a sustained high-risk period as teens engage in more extensive outdoor pursuits including camping trips, wilderness exploration, competitive outdoor sports, and social activities in wooded or grassy areas. The bimodal distribution pattern characteristic of Lyme disease shows teens occupying the first major peak, while adults aged 45-54 represent the second peak, reflecting different patterns of environmental exposure across the lifespan. The persistent gender disparity, with male teens experiencing higher incidence rates, aligns with behavioral research showing boys typically spend more time in high-risk wooded and grassy environments compared to girls. However, the substantial number of cases among female teenagers demonstrates that Lyme disease remains a significant health threat across all adolescent demographics regardless of gender.
Geographic Distribution of Lyme Disease in Teens Across the US 2023
| State | Annual Cases 2022 | Rate per 100,000 | Teen Risk Level |
|---|---|---|---|
| Pennsylvania | 8,413 cases | Highest nationwide | Extremely High |
| New Jersey | 5,900 cases | 69.1 per 100,000 (2023 average) | Extremely High |
| New York | 2,018 cases | High incidence | Very High |
| Connecticut | 2,718 average annually | Lower than NE average | High |
| Maine | 2,653 cases | 192.6 per 100,000 | Very High |
| Rhode Island | Highest rate 2022 | Highest per capita | Very High |
| Vermont | Second highest rate | Very high per capita | Very High |
| High-incidence states | 15 states total | 95.5% of all cases | High to Extremely High |
| Middle Atlantic region | 56,000+ four-year total | 56% of national cases | Extremely High |
| New England region | 18,000+ four-year total | Second highest burden | Very High |
Data Source: CDC Lyme Disease Surveillance 2022-2023; State Health Departments; Spotlight PA; CT Mirror 2025
The geographic distribution of Lyme disease cases reveals stark regional disparities that directly impact teenage populations across America. Pennsylvania reported 8,413 confirmed cases in 2022, representing nearly one-third of all confirmed national cases and making it the epicenter of Lyme disease transmission affecting teens. Pennsylvania has maintained the highest incidence rate nationwide for 11 of the past 12 years, creating an environment where Pennsylvania teens face extraordinarily elevated infection risks compared to adolescents in other states. New Jersey, with the fourth-most reported cases nationally in 2023, demonstrated an average incidence of 69.1 cases per 100,000 population, while Rhode Island, Vermont, and Maine had the highest rates per capita in 2022.
The concentration of 95.5% of cases in just 15 high-incidence states creates dramatically different risk profiles for teenagers depending on their state of residence. The Middle Atlantic region, including New Jersey, New York, and Pennsylvania, accounts for more than half of nationwide cases during analyzed periods, making this tri-state area particularly hazardous for adolescent outdoor activities. Teens living in these endemic regions face daily exposure risks that their counterparts in low-incidence states rarely encounter. Recent surveillance from Dartmouth found that half of all adult blacklegged ticks in the Northeast carry Lyme-causing bacteria, with up to 25% of harder-to-detect nymph-stage ticks also infected. This extraordinarily high infection prevalence among tick populations means that teenagers in endemic states who spend time outdoors face roughly a one-in-two chance of encountering an infected tick during peak season, underscoring why geographic targeting of prevention education and the Lambert High School CRISPR diagnostic breakthrough matter so profoundly for protecting adolescent health.
Breakthrough Teen Innovation in Lyme Disease Detection in the US 2025
| Innovation Category | Details | Impact |
|---|---|---|
| Developer Team | Lambert High School students, Georgia | Teenage genetic engineers |
| Technology Used | CRISPR gene editing | Synthetic biology application |
| Detection Window | 2 days post-infection | Revolutionary early detection |
| Current Test Limitation | 14+ days required | Standard antibody tests |
| Competition | iGEM Paris 2025 | International Genetically Engineered Machine |
| Team Captains | Sean Lee and Avani Karthik | High school seniors |
| Potential Impact | Millions of people | Nationwide health transformation |
| Diagnostic Gap Addressed | Early detection failure | Solves decades-old problem |
| Undiagnosed Cases | 15 years without diagnosis | Patients team encountered |
| Scientific Validation | Further testing needed | Potential major breakthrough |
| Field of Work | Synthetic biology | Biology, engineering, genetics, computer science |
| Problem Solved | Real-world application | Practical health solution |
Data Source: CBS News 60 Minutes, November 30, 2025
In November 2025, a remarkable development emerged that could fundamentally transform Lyme disease diagnosis for teenagers and all Americans. A team of public high school students at Lambert High School in suburban Atlanta, Georgia, accomplished what adult scientists have struggled to achieve for decades by developing a CRISPR-based diagnostic test capable of detecting Lyme disease just two days after infection. This breakthrough stands in stark contrast to current antibody testing methods that require waiting two weeks or longer before providing accurate results, creating a critical diagnostic gap during the period when antibiotic treatment proves most effective. High school senior Claire Lee captured the magnitude of their achievement, stating their work in a high school lab could potentially have a huge impact for millions of people and help save lives.
The Lambert team, led by team captains Sean Lee and Avani Karthik, utilized synthetic biology combining biology with engineering, genetics, and computer science to address one of Lyme disease’s most persistent challenges. Team member Avani Karthik emphasized that one of the biggest problems with Lyme disease is the lack of early diagnostic capability, noting they met someone who went 15 years without a diagnosis due to testing limitations. The students competed at the iGEM competition in Paris, essentially a science Olympics where teams must use synthetic biology to solve real-world problems. Scientists now say the students’ groundbreaking work could represent a major breakthrough if further testing validates their approach. For the estimated 476,000 Americans diagnosed and treated for Lyme disease annually, including thousands of teenagers, this innovation could prevent the 60% arthritis risk, 15% neurologic complications, and cardiac problems that plague patients who cannot access early treatment due to current diagnostic limitations during the critical first two weeks of infection.
Clinical Manifestations of Lyme Disease in Teens in the US 2023
| Symptom Category | Presentation | Frequency in Teens | Timing |
|---|---|---|---|
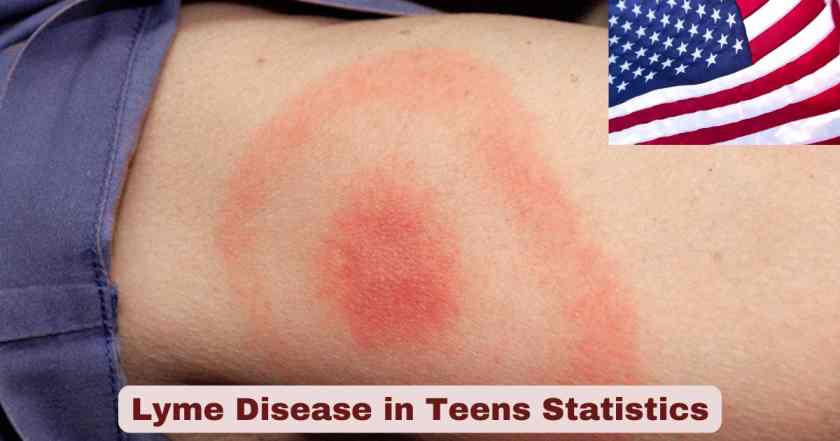
| Erythema Migrans rash | Bull’s-eye pattern | 70-80% of cases | 3-30 days post-bite |
| Fever | Low-grade to moderate | Common | Early infection |
| Headache | Persistent | Very common | Early to disseminated |
| Fatigue | Extreme tiredness | Very common | All stages |
| Muscle aches | Myalgia | Common | Early infection |
| Joint pain | Arthralgia | Common | Early to late stages |
| Stiff neck | Neck rigidity | Moderate | Neurological involvement |
| Lyme arthritis | Knee swelling primarily | 60% if untreated | Weeks to months |
| Neurologic symptoms | Facial palsy, meningitis | 15% if untreated | Weeks to months |
| Cardiac involvement | Heart block | 4-10% historical | Weeks after infection |
| Cognitive issues | Memory, concentration | Present in some | Late-stage disease |
| Bell’s palsy | Facial drooping | Can occur in teens | Disseminated infection |
Data Source: CDC Clinical Information; Medical Literature 2022-2023
The clinical manifestations of Lyme disease in teenagers follow predictable patterns that parents, healthcare providers, and teens themselves must recognize for prompt treatment. The characteristic erythema migrans rash, often appearing as a bull’s-eye pattern at the tick bite site, develops in 70-80% of cases between 3-30 days after infection. However, the concerning reality remains that 20-30% of infected teens never develop this telltale rash, making diagnosis challenging and highlighting why the Lambert High School CRISPR test breakthrough matters tremendously. Early symptoms including fever, headache, extreme fatigue, and muscle aches often mimic common viral illnesses, leading to potential misdiagnosis during the critical early treatment window when antibiotics work most effectively.
Without early detection and treatment, Lyme disease progresses to disseminated and late-stage infections causing serious complications that can permanently impact teenagers’ health and quality of life. The statistic showing 60% of untreated patients develop Lyme arthritis, primarily affecting the knees with painful swelling and limited mobility, represents a devastating outcome for active adolescents engaged in sports, physical education, and normal teenage activities. Neurological manifestations occurring in 15% of untreated cases can include facial palsy, meningitis, cognitive difficulties affecting academic performance, and memory problems that interfere with school success during critical educational years. The 4-10% historical rate of cardiac involvement, while reduced with modern early treatment practices, can cause heart block requiring hospitalization and potentially life-threatening complications. These severe outcomes underscore why current diagnostic delays of two weeks or longer with standard antibody tests create unacceptable risks, making innovations in early detection not merely scientific curiosities but urgent medical necessities for protecting teenage health across endemic regions where hundreds of thousands face annual exposure risks.
Risk Factors and Outdoor Activities Affecting Teens in the US 2023
| Risk Factor | Details | Teen Exposure Level |
|---|---|---|
| Outdoor recreation | Hiking, camping, trail activities | Very High |
| Sports participation | Soccer, cross-country, outdoor athletics | High |
| Backyard exposure | 50% of PA tick bites | Very High |
| Time of year | June-July peak season | Highest exposure |
| Geographic location | Northeast, Mid-Atlantic, upper Midwest | Endemic regions |
| Wooded areas | Forest environments | Very High |
| Grassy areas | Tall grass, brush | High |
| Male gender | Higher outdoor activity time | Elevated risk |
| Tick season extension | Climate change impact | Year-round possibility |
| Temperature threshold | Above 45°F tick activity | Extended season |
| Forest fragmentation | Development in tick habitat | Increased human contact |
| Deer population | Primary adult tick host | High in endemic areas |
Data Source: CDC Risk Factors; East Stroudsburg University Tick Lab; Penn State Research 2023-2024
Multiple interconnected risk factors elevate Lyme disease transmission among American teenagers, with outdoor recreational activities representing the primary exposure pathway. Adolescents engage in hiking, camping, trail running, and wilderness exploration at higher rates than many other age groups, placing them in direct contact with blacklegged tick habitats during peak activity seasons. Sports participation, particularly soccer, cross-country running, lacrosse, and other outdoor athletics, frequently occurs in grassy fields and wooded areas where tick populations thrive. Perhaps most surprisingly, 50% of Pennsylvania tick bites occur in backyards, revealing that teens don’t need to venture into wilderness areas to face substantial infection risks in endemic regions.
Temporal and environmental factors compound these activity-based risks for teenage populations. Lyme disease cases peak during June and July when people encounter ticks most frequently, coinciding precisely with summer vacation when teenagers spend maximum time outdoors without school constraints. Climate change has extended tick season significantly, with ticks becoming active year-round when temperatures exceed 45°F, creating exposure opportunities even during mild winter periods when teens might not expect tick-borne disease risks. Forest fragmentation from residential and commercial development increases human-tick contact by bringing suburban homes and teen gathering spaces directly into traditional tick habitats. As forests are cleared for housing developments and shopping centers where teenagers congregate, displaced ticks remain in place and increasingly bite humans rather than their natural wildlife hosts. The combination of male teenagers spending more time in high-risk environments, geographic residence in 15 high-incidence states containing 95.5% of all cases, and extended tick activity seasons creates a perfect storm of risk factors that expose hundreds of thousands of American teens to potential Lyme infection annually.
Treatment Protocols and Recovery Outcomes for Teens in the US 2023
| Treatment Category | Protocol | Duration | Success Rate |
|---|---|---|---|
| Early localized infection | Doxycycline (first-line) | 10-21 days | Excellent recovery |
| Alternative antibiotic | Amoxicillin | 14-21 days | High effectiveness |
| Alternative antibiotic | Cefuroxime | 14-21 days | High effectiveness |
| Neurologic Lyme | IV ceftriaxone | 14-28 days | Good with early treatment |
| Lyme arthritis | Oral antibiotics (extended) | 28 days | Most resolve |
| Cardiac Lyme | IV antibiotics, monitoring | 14-21 days | Requires hospitalization |
| Early treatment benefit | Prevents complications | Critical first 14 days | Near-complete recovery |
| Delayed treatment | Persistent symptoms possible | Variable | More complications |
| Post-treatment symptoms | Fatigue, pain | Months | Gradual improvement |
| Retreatment | Sometimes necessary | Additional courses | Case-dependent |
| Doxycycline age minimum | 8 years and older | Standard duration | Preferred for teens |
| Recovery with early Rx | Full recovery | Weeks to months | Majority of teens |
Data Source: CDC Treatment Guidelines; Infectious Diseases Society of America 2023
Treatment outcomes for Lyme disease in teenagers depend critically on how quickly diagnosis occurs and antibiotic therapy begins, making the Lambert High School CRISPR breakthrough potentially transformative for adolescent health outcomes. For early localized infection detected within the first weeks, doxycycline serves as the first-line antibiotic treatment for teens aged 8 years and older, administered for 10-21 days depending on clinical presentation. Alternative antibiotics including amoxicillin and cefuroxime provide effective options for teens with doxycycline contraindications or younger children. When treatment begins during early infection before dissemination occurs, recovery rates approach near-complete with most teens experiencing full resolution of symptoms within weeks to months.
The stark contrast between early and delayed treatment outcomes explains why current diagnostic limitations causing two-week or longer waits for accurate test results create such serious health consequences. Disseminated infections requiring more aggressive interventions include neurologic Lyme treated with IV ceftriaxone for 14-28 days, Lyme arthritis managed with extended oral antibiotic courses of 28 days, and cardiac Lyme necessitating hospitalization with IV antibiotics and cardiac monitoring. While most teens recover even from these complications when properly treated, some experience persistent post-treatment symptoms including fatigue, pain, and cognitive difficulties lasting months beyond antibiotic completion. The 60% arthritis risk and 15% neurologic complication rate among untreated patients demonstrates the devastating consequences when diagnosis delays prevent timely antibiotic intervention. These statistics emphasize why innovations enabling detection as early as two days post-infection, compared to current 14+ day waits, could prevent thousands of teenagers annually from progressing beyond easily treatable early infection to complicated disseminated disease requiring intensive medical management and potentially causing permanent health impacts.
Prevention Strategies for Teenagers in the US 2025
| Prevention Method | Implementation | Effectiveness | Teen Compliance |
|---|---|---|---|
| Insect repellent use | EPA-registered products with DEET | High | Variable |
| Permethrin on clothing | Treat clothes, boots, camping gear | Very High | Low without parental involvement |
| Protective clothing | Long sleeves, long pants | Moderate-High | Low in summer heat |
| Light-colored clothing | Makes ticks visible | Aids detection | Moderate |
| Tuck pants into socks | Physical barrier | High | Very Low |
| Walk in trail centers | Avoid brush contact | Moderate | Moderate with education |
| Tick checks after outdoors | Full body inspection | Very High | Low without reminders |
| Showering within 2 hours | Washes off unattached ticks | High | Moderate |
| Yard maintenance | Mow lawns, clear brush, remove leaves | High | Requires parental action |
| Create tick-safe zones | Wood chips, gravel barriers | Moderate | Parental implementation |
| Avoid tick habitats | Limit wooded/grassy area time | High | Very Low (unrealistic) |
| Tick removal tools | Fine-tipped tweezers | Critical when bitten | Requires education |
Data Source: CDC Prevention Guidelines; New Jersey Department of Health 2024; Medical Recommendations 2023
Effective Lyme disease prevention for teenagers requires multi-layered approaches addressing both personal protective behaviors and environmental modifications, though compliance challenges persist across this age group. Personal protective measures start with applying EPA-registered insect repellents containing DEET to exposed skin before outdoor activities, though teenage compliance remains inconsistent without parental supervision and reminders. Treating clothing, boots, and camping gear with permethrin provides highly effective protection by killing ticks on contact, but this measure typically requires parental involvement as few teens independently treat their gear. Wearing protective clothing including long sleeves and pants tucked into socks offers physical barriers against tick attachment, but teenage compliance plummets during hot summer months when comfort takes priority over prevention despite this being peak tick season.
Environmental and behavioral modifications provide additional protective layers when personal measures fail. Maintaining yards by mowing lawns regularly, clearing brush, and removing leaf litter eliminates tick habitats near homes where 50% of Pennsylvania tick bites occur. Walking in the center of trails rather than allowing contact with bordering vegetation reduces tick encounters during hiking and outdoor recreation. Performing full-body tick checks after outdoor activities and showering within 2 hours of coming indoors proves highly effective at removing unattached ticks before they bite, but teenagers often skip these crucial steps without parental enforcement. The compliance challenge becomes particularly acute because effective prevention requires consistent implementation of multiple measures simultaneously – using repellents, wearing protective clothing, performing tick checks, and showering promptly – when adolescents typically prioritize convenience and social norms over health precautions. This prevention gap, combined with the two-week diagnostic window of current tests, creates circumstances where thousands of teenagers annually contract Lyme disease despite available protective measures, reinforcing why early detection innovations like the Lambert High School CRISPR test detecting infection within 2 days could transform outcomes even when prevention efforts fail.
Long-Term Health Implications for Teens in the US 2023
| Complication | Prevalence | Impact on Teens | Duration |
|---|---|---|---|
| Lyme arthritis | 60% if untreated | Knee swelling, limited mobility, sports impact | Months to years |
| Joint damage | Chronic cases | Permanent cartilage damage possible | Potentially lifelong |
| Neurologic problems | 15% if untreated | Cognitive issues, academic performance decline | Variable |
| Memory difficulties | Post-Lyme subset | School performance, standardized testing impact | Months to years |
| Concentration problems | Post-treatment possible | Academic challenges, focus issues | Weeks to months |
| Chronic fatigue | Common in delayed treatment | Limits physical activity, social participation | Months to years |
| Facial palsy | Neurologic Lyme | Social stigma, psychological impact | Usually resolves |
| Cardiac complications | 4-10% historical | Heart block, exercise limitation | Typically resolves |
| Post-treatment syndrome | 10-20% of patients | Persistent symptoms after treatment | 6+ months |
| Psychological impact | Chronic illness | Anxiety, depression, social isolation | Variable |
| Academic disruption | Severe cases | Missed school, reduced participation | Weeks to months |
| Athletic participation | Arthritis/fatigue | Sports cessation, reduced fitness | Season to permanent |
Data Source: CDC Clinical Outcomes; Medical Literature 2022-2023; Patient Studies
The long-term health implications of Lyme disease prove particularly devastating for teenagers during critical developmental years when physical activity, academic achievement, and social development shape future life trajectories. Lyme arthritis affecting 60% of untreated patients predominantly impacts knees with painful swelling that can last months to years, forcing athletic teens to abandon sports seasons or permanently quit teams when treatment delays allow progression to chronic joint inflammation. For teenagers whose identities center around athletic achievement or whose college prospects depend on continued sports participation, losing entire seasons or careers to preventable Lyme complications creates profound psychological and practical consequences extending far beyond immediate physical symptoms.
Neurological and cognitive complications affecting 15% of untreated cases strike at the core of teenage academic responsibilities and social functioning. Memory difficulties interfere with learning new material, studying for examinations, and retaining information for standardized tests that determine college admissions. Concentration problems make completing homework assignments, focusing during classes, and participating in extracurricular activities increasingly difficult when teens need peak cognitive performance. Chronic fatigue persisting months after treatment completion limits participation in social activities, reduces energy for maintaining friendships, and contributes to social isolation during years when peer relationships profoundly influence psychological development. Post-treatment Lyme disease syndrome affecting 10-20% of patients with symptoms lasting 6+ months creates ongoing disability during prime teenage years that should involve exploration, growth, and preparation for adult independence. These long-term complications, largely preventable through early diagnosis and treatment, underscore why current diagnostic delays of 14+ days cause unacceptable harm and why breakthrough innovations like the Lambert High School students’ 2-day CRISPR detection method represent not merely scientific achievements but urgent medical necessities for protecting hundreds of thousands of American teenagers facing annual Lyme disease exposure risks in endemic regions across the United States.
Disclaimer: This research report is compiled from publicly available sources. While reasonable efforts have been made to ensure accuracy, no representation or warranty, express or implied, is given as to the completeness or reliability of the information. We accept no liability for any errors, omissions, losses, or damages of any kind arising from the use of this report.